Neurological disorders are conditions that affect the brain, spinal cord, and nerves—impacting everything from how we move and think to how we feel and function. These disorders range from mild to life-altering and include well-known conditions like migraines, epilepsy, Alzheimer’s disease, multiple sclerosis (MS), and Parkinson’s disease.
Today, millions of people worldwide live with neurological conditions, making them a major concern in public health. In fact, neurological disorders are among the leading causes of disability and death globally. They affect people of all ages, but their impact grows significantly with age.
What makes these conditions especially challenging is that symptoms can be subtle in the beginning—such as mild memory loss or numbness in a limb—and are often mistaken for other issues. That’s why early recognition and proper management are so critical. The sooner a neurological disorder is identified, the better the chances of managing symptoms, slowing progression, and improving quality of life.
In this article, we’ll explore the most common neurological disorders, what causes them, how they’re diagnosed, and the steps you can take to manage or prevent them.
What Are Neurological Disorders?
Neurological disorders are medical conditions that affect the central and peripheral nervous systems, including the brain, spinal cord, and nerves. These systems control nearly every function in the body—from muscle movement and sensation to memory, mood, and cognition. When something goes wrong in the nervous system, the effects can be wide-ranging and often life-changing.
There are many types of neurological conditions, including chronic diseases like multiple sclerosis, progressive disorders such as Parkinson’s and Alzheimer’s, and acute events like stroke or traumatic brain injury. Some neurological disorders are inherited, while others result from infections, autoimmune reactions, tumors, traumatic injuries, or simply age-related degeneration.
A 2022 report published in The Lancet Neurology emphasized that neurological conditions now represent a leading cause of disability-adjusted life years (DALYs) worldwide—highlighting the urgent need for early diagnosis and treatment.
Symptoms vary depending on the part of the nervous system involved. They can include pain, weakness, numbness, memory loss, seizures, difficulty speaking or walking, and changes in mood or behavior. Some conditions are stable, while others may worsen over time if not properly managed.
Understanding what neurological disorders are is the first step in recognizing them early and seeking appropriate medical care. Timely intervention can improve outcomes, preserve function, and enhance quality of life.
Top 10 Most Common Neurological Disorders
Neurological disorders are among the leading causes of disability worldwide, affecting people of all ages. They impact the brain, spinal cord, and peripheral nerves, often disrupting movement, memory, speech, sensation, and cognition. According to the World Health Organization (WHO), neurological conditions affect over 1 billion people globally. Below is a detailed look at ten of the most common and clinically significant types of neurological disorders, including their symptoms, causes, and current treatment strategies.
1. Alzheimer’s Disease
Alzheimer’s disease is the most common cause of dementia, responsible for up to 70% of dementia cases.
Symptoms:
- Gradual memory loss
- Disorientation in familiar environments
- Trouble finding words and following conversations
- Personality changes and confusion
Causes:
- Accumulation of beta-amyloid plaques and tau tangles in the brain
- Genetic factors (e.g., APOE-e4 allele)
- Age is the strongest risk factor
Treatment:
- No cure, but FDA-approved drugs like donepezil, galantamine, and memantine may slow cognitive decline
- Lifestyle interventions (e.g., physical activity, social engagement) are recommended
- Aducanumab and lecanemab target amyloid plaques (used in select patients)
>>Related: How Alzheimer’s Disease Is Diagnosed
2. Parkinson’s Disease
Parkinson’s disease (PD) is a progressive neurodegenerative disorder affecting motor control. It affects over 10 million people worldwide.
Symptoms:
- Resting tremor, especially in hands
- Muscle rigidity
- Bradykinesia (slowness of movement)
- Postural instability and frequent falls
- “Mask-like” facial expression
Causes:
- Loss of dopamine-producing neurons in the substantia nigra (midbrain)
- Genetic mutations (e.g., LRRK2, PARK7)
- Environmental toxins like pesticides may increase risk
Treatment:
- Levodopa (mainstay therapy), dopamine agonists, MAO-B inhibitors
- Deep brain stimulation (DBS) for advanced stages
- Speech and physical therapy improve function
3. Stroke
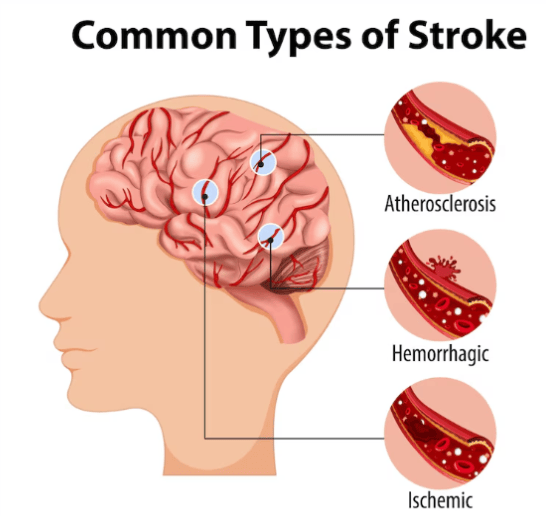
A stroke occurs when blood supply to part of the brain is interrupted or reduced. Every 40 seconds, someone in the U.S. has a stroke, making it a leading cause of serious long-term disability.
Symptoms:
- Sudden weakness or numbness (especially on one side)
- Trouble speaking or understanding speech
- Vision problems
- Loss of balance or coordination
- Sudden severe headache (hemorrhagic stroke)
Causes:
- Ischemic stroke (87% of cases): blocked artery due to a clot
- Hemorrhagic stroke: rupture of a blood vessel in the brain
- Risk factors: hypertension, atrial fibrillation, diabetes, smoking
Treatment:
- Immediate administration of clot-busting drugs (tPA) within 3–4.5 hours
- Thrombectomy for large clots
- Long-term: blood pressure control, antiplatelet therapy, rehabilitation
4. Epilepsy
Epilepsy is a neurological disorder characterized by recurrent, unprovoked seizures due to abnormal electrical activity in the brain.
Symptoms:
- Focal or generalized seizures
- Convulsions, loss of consciousness
- Sensory changes (smell, sound, vision)
- Behavioral and mood changes
Causes:
- Genetic predisposition
- Brain injury, infections (e.g., meningitis), stroke, tumors
- Unknown in nearly 50% of cases (idiopathic)
Treatment:
- Anti-epileptic drugs (AEDs): carbamazepine, lamotrigine, levetiracetam
- Vagus nerve stimulation (VNS), ketogenic diet for refractory epilepsy
- Surgical resection in drug-resistant cases
5. Migraine
Migraines are disabling, recurrent headaches often associated with nausea and sensory sensitivities. They affect more than 1 in 7 people globally, and are three times more common in women.
Symptoms:
- Throbbing headache (usually one-sided)
- Nausea, vomiting
- Sensitivity to light and sound
- Aura (visual disturbances, tingling, speech difficulty)
Causes:
- Genetic predisposition (familial migraine)
- Hormonal changes, stress, sleep disruption, dietary triggers
Treatment:
- Acute: NSAIDs, triptans, gepants
- Preventive: beta-blockers, topiramate, CGRP inhibitors (e.g., erenumab)
- Lifestyle modifications: hydration, regular sleep, identifying triggers
6. Multiple Sclerosis (MS)
MS is an autoimmune condition where the immune system attacks the myelin sheath of nerve fibers in the brain and spinal cord. It typically presents between ages 20 and 40.
Symptoms:
- Fatigue, vision changes (optic neuritis)
- Tingling, numbness, and muscle weakness
- Difficulty with balance, walking, and coordination
- Cognitive fog and mood swings
Causes:
- Unknown, but linked to genetics, Epstein-Barr virus (EBV), and low vitamin D
- More common in women and people of Northern European descent
Treatment:
- Disease-modifying therapies (DMTs): ocrelizumab, fingolimod, interferons
- Corticosteroids for acute flare-ups
- Rehabilitation and symptom-specific treatments
7. Peripheral Neuropathy
Peripheral neuropathy refers to damage of peripheral nerves, especially in the hands and feet. It affects up to 50% of people with long-standing diabetes.
Symptoms:
- Burning, tingling, or numbness
- Sharp, stabbing pain
- Loss of balance or reflexes
- Muscle weakness
Causes:
- Diabetes (most common), alcohol abuse, infections, vitamin B12 deficiency, chemotherapy, autoimmune diseases
Treatment:
- Blood sugar control for diabetic neuropathy
- Pain management: duloxetine, gabapentin, pregabalin
- Addressing underlying cause, physical therapy
8. ALS (Amyotrophic Lateral Sclerosis)
ALS is a progressive disease affecting motor neurons, causing loss of voluntary muscle movement and eventually leading to respiratory failure.
Symptoms:
- Muscle twitching and cramping
- Weakness in arms or legs
- Slurred speech, difficulty swallowing
- Shortness of breath
Causes:
- 90–95% are sporadic; ~5–10% familial (e.g., SOD1 mutation)
- Environmental exposures and military service have been linked
Treatment:
- Riluzole and edaravone to modestly slow progression
- Multidisciplinary care: physical, occupational, and respiratory therapy
- Mechanical ventilation and nutritional support in late stages
9. Autism Spectrum Disorders (ASD)
ASD encompasses a group of neurodevelopmental disorders affecting social interaction, communication, and behavior. Prevalence in the U.S. is estimated at 1 in 36 children (CDC, 2023).
Symptoms:
- Delayed speech and language skills
- Repetitive behaviors or restricted interests
- Social withdrawal, difficulty with eye contact
- Sensory sensitivities
Causes:
- Largely genetic; potential link to prenatal factors and advanced parental age
- Not caused by vaccines (confirmed by multiple large-scale studies)
Treatment:
- Early behavioral intervention (ABA), speech and occupational therapy
- Special education support
- No medications for core symptoms, but adjuncts used for irritability or anxiety
10. Head Injuries and Concussions
Traumatic Brain Injury (TBI) results from external force causing brain dysfunction. Mild forms like concussions are common but can have long-term effects if repeated or untreated.
Symptoms:
- Headache, confusion, memory loss
- Nausea, dizziness, vision problems
- Mood changes, sleep disruption
Causes:
- Falls, car accidents, sports injuries, violence
- Repeated concussions linked to chronic traumatic encephalopathy (CTE)
Treatment:
- Rest, symptom management, gradual return to activity
- Cognitive rehab and counseling in persistent cases
- Helmets and safety measures can prevent many TBIs
These common neurological disorders vary in onset, severity, and treatment needs—but they all require timely attention. Understanding brain disease symptoms and knowing when to seek professional evaluation empowers patients and families to take control of their neurological health.
Causes and Risk Factors for Neurological Disorders
Neurological conditions can develop for a variety of reasons—some we can control, and others we can’t. Understanding the causes of neurological disorders and identifying key risk factors for brain conditions is essential for both prevention and early detection.
Non-Modifiable Risk Factors
- Aging is one of the most significant risk factors. As we age, brain cells naturally decline in function and number, making conditions like Alzheimer’s and Parkinson’s more common.
- Genetics can also play a major role. Family history of certain disorders, such as epilepsy or Huntington’s disease, increases individual risk.
- Some neurological conditions are triggered by autoimmune responses—where the immune system mistakenly attacks the nervous system, as seen in multiple sclerosis.
Modifiable Lifestyle Factors
- Smoking, poor diet, and physical inactivity are linked to increased risk of stroke, vascular dementia, and neuropathy.
- Uncontrolled diabetes, high blood pressure, and obesity further strain the brain and nervous system over time.
- Alcohol and drug misuse can damage nerve tissue and interfere with neurotransmitter function.
Other Contributing Factors
- Infections such as meningitis, HIV, or Lyme disease can inflame or damage the brain and nerves.
- Environmental exposures to heavy metals, pesticides, or industrial chemicals may increase long-term neurological risks.
- Traumatic brain injuries (TBIs) from falls, accidents, or sports are a known trigger for both immediate and delayed neurological symptoms.
While not all causes can be avoided, managing the risk factors within your control—like diet, exercise, and safety—can go a long way in protecting your brain and nervous system.
When to See a Neurologist
Many people ignore early signs of brain or nerve problems, hoping they’ll go away. But when it comes to the nervous system, early attention can make all the difference. Recognizing the symptoms of neurological illness and knowing when to see a neurologist can lead to faster diagnosis and better outcomes.
Warning Signs You Shouldn’t Ignore
You should consult a neurologist if you experience:
- Frequent or severe headaches that don’t improve with medication
- Numbness or tingling in your arms, legs, or face
- Muscle weakness or coordination problems
- Unexplained confusion, memory loss, or personality changes
- Double vision, blurry sight, or sudden vision loss
- Seizures, dizziness, or difficulty speaking
These symptoms could point to underlying conditions like migraines, stroke, multiple sclerosis, or even early signs of dementia.
Why Early Evaluation Matters
Neurologists are trained to evaluate, diagnose, and manage disorders of the brain, spine, and nerves. Getting help early can prevent long-term damage, slow disease progression, and improve your quality of life. A neurologist may recommend testing, imaging, medications, or therapy depending on your condition.
Don’t wait until symptoms worsen. If something feels off with your nervous system, getting it checked sooner rather than later is always the smarter move.
Neurological Disorders: Frequently Asked Questions
Are neurological disorders curable?
Some neurological disorders are curable, while others are chronic and require long-term management. For example, certain infections or migraines may be treated completely, while conditions like Parkinson’s, Alzheimer’s, or multiple sclerosis are managed with medications and therapies to slow progression and improve quality of life.
What’s the difference between neurological and psychiatric disorders?
Neurological disorders are caused by structural or biochemical issues in the nervous system—like nerve damage or brain inflammation. Psychiatric disorders, such as anxiety or depression, primarily involve mood, thought, or behavior but can overlap with neurological symptoms. A neurologist or psychiatrist can help distinguish between the two.
Can stress cause neurological symptoms?
Yes. Chronic stress can lead to headaches, muscle tension, dizziness, memory problems, and even numbness or tingling. While stress doesn’t directly cause diseases like ALS or MS, it can worsen symptoms and affect how your nervous system functions.
How are neurological diseases diagnosed?
Diagnosis usually involves a neurological exam, imaging (like MRI or CT scans), blood tests, and sometimes nerve conduction studies or spinal fluid analysis. The process helps rule out other conditions and pinpoint the cause of your symptoms.
Conclusion
Neurological disorders may sound overwhelming, but with early diagnosis and proper care, many can be managed effectively. From migraines and epilepsy to conditions like Parkinson’s and dementia, recognizing the warning signs early gives you the best chance at slowing progression and preserving quality of life.
Awareness is the first step. If you or someone you love experiences symptoms like numbness, confusion, or frequent headaches, don’t ignore them. Seeking help from a neurologist can lead to timely treatment, accurate diagnosis, and better outcomes.
By staying informed about common neurological disorders and taking action when symptoms appear, you’re actively supporting your neurological health—and that matters at every age.